Dr Sultan Linjawi
MBBS BSc MRCP (UK) FRACP
Brisbane
Toowoomba
T: 07 3737 7896
F: 07 3102 9927
E: drSlinjawi@gmail.com
Dr Sultan Linjawi
MBBS BSc MRCP (UK) FRACP
Brisbane
Toowoomba
T: 07 3737 7896
F: 07 3102 9927
E: drSlinjawi@gmail.com
Call for Appointments
07 3737 7896
Call for Appointments
07 3737 7896

What is Type 2 Diabetes?
Type 2 diabetes explained simply
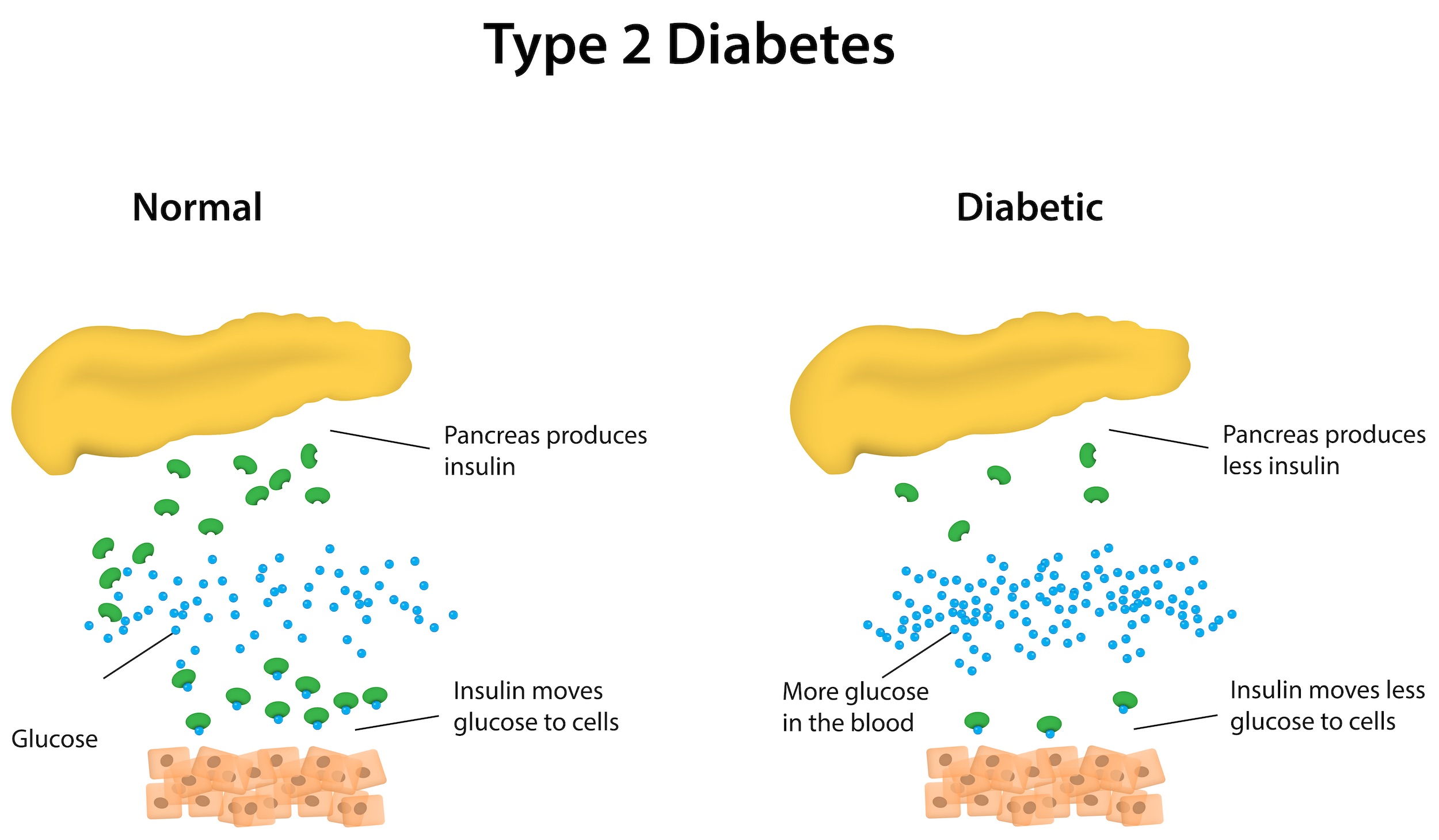
Type 2 diabetes is an elevation in blood sugars that occurs when a sugar called glucose can’t get into your fat and muscles where it is needed. Elevated blood glucose damages the lining of blood vessels leading to a range of complications in various organs of the body.
Type 2 diabetes explained in more detail
Type 2 diabetes is rapidly becoming one of the most common long-term disease in the world. The problem causing an elevation in the blood glucose levels occurs when there is a change in the shape of the insulin receptor. In the normal situation, the body produces a small chemical called insulin (key) whose purpose is to bind to a receptor (lock) on the surface of fat and muscle cells, opening a channel to allow glucose to enter those cells. In type 2 diabetes the shape of this receptor changes mostly as a consequence of weight gain around the stomach. The process of the lock changing shape is called Insulin Resistance (see video below).
Type 2 diabetes mellitus is a very serious condition
The number of people diagnosed with diabetes is increasing. The 8th edition of the International Diabetes Federation’s (IDF) Diabetes Atlas released in 2017, estimated that:
- One in 11 people have diabetes (425 million)
- One in two adults with diabetes are undiagnosed (212 million)
- 12% of global health expenditure is spent on diabetes (USD$727 billion)
- Every 6 seconds a person dies from diabetes

People with diabetes who have ongoing high blood glucose levels, are at an increased risk of having poor health outcomes compared to people who do not have diabetes. This includes:
- People with diabetes are up to four time more likely to suffer heart attacks or strokes
- Diabetes is the leading cause of vision-loss globally and is the fifth most common cause of preventable blindness and fifth more common cause of moderate to severe visual impairment
- Kidney failure is three times more common in people with diabetes
- Amputations are 15 times more common in people with diabetes
- More than 30 percent of people with diabetes experience depression, anxiety, and distress
Early diagnosis, optimal treatment, and effective ongoing support and management can reduce the risk of diabetes-related complications dramatically.
Who is at risk of developing type 2 diabetes?
Risk factors can be divided into non-modifiable risk factors and modifiable risk factors. Non-modifiable risk factors are those that can’t be changed by you, for example your genetics. Modifiable risk factors can be changed, for example making changes to the amount you exercise.

Non-modifiable risk factors in type 2 diabetes?
The non-modifiable risk factors which increase your chance of developing prediabetes include:
- Have a family history of diabetes
- Being older (over 55 years of age) – the risk increases as we age
- Ethnic background, including Aboriginal and Torres Strait Islanders, Pacific Islanders, Asian and South East Asian, African Americans, Native Hawaiians, and Hispanics/ Latinos
Being aware of the non-modifiable risk factors is extremely important. For people who have a family history of type 2 diabetes, you need to be more alert and start taking action early to prevent or delay developing type 2 diabetes.
Modifiable risk factors in type 2 diabetes
The modifiable risk factors which increase your chance of developing prediabetes include:
- Being overweight or obese, particularly extra weight around the waist
- Being physically inactive
- Eating a poor diet (one that is high in fat, salt, and sugar)
- High blood pressure
Are there other risk factors?
There are some risk factors that cross over between modifiable and non-modifiable risk factors. Some of these include:
- Having signs associated with diabetes like skin tags and dark colouration around the neck and arm pits called acanthosis nigricans
- Over 45 years of age and being overweight
What are the symptoms of type 2 diabetes?
This might come as a shock to you, but the most common symptoms of type 2 diabetes mellitus is nothing at all. That’s part of the problem; the person feels ok, but the damage is already occurring. Many people experience tiredness and fatigue and that is really noticed when you start to get sugars under more control. When the blood sugar levels are grossly elevated then people may notice excessive thirst and trips to the toilet to pass urine. This occurs as high blood sugars pass into the urine and with the sugar, goes water.
Diabetes symptoms that could affect anyone
The general symptoms and signs of type 2 diabetes include:
- Fatigue and irritability
- Excessive thirst, frequent urination, and dehydration
- Ongoing hunger
- Yeast and bacterial infections
- Dry and itchy skin
- Cuts and wounds that don’t heal quickly
- Pain and numbness in your feet or legs
- Blurred vision
- Changes in weight
Type 2 diabetes symptoms in men
There are some symptoms of type 2 diabetes mellitus in men and are often related to sexual health and function.
- Erectile dysfunction
- Retrograde ejaculation
- Urologic issues, including overactive bladder, urinary tract infections, and inability to control urination
- Decreased sex drive
Type 2 diabetes symptoms in women
The symptoms of type 2 diabetes in women also often relate to sexual health and function. They include:
- Vaginal and oral yeast infections, and vaginal thrush
- Urinary tract infections
- Female sexual dysfunction
- Polycystic ovary syndrome
How is type 2 diabetes diagnosed?
Most people diagnosed with diabetes are picked up by chance based on a high blood glucose levels noticed in routine testing. This is not the best way to test for diabetes and more formal and targeted tests should be asked for.
Tests used to diagnose type 2 diabetes include the random blood glucose test, oral glucose tolerance test, fasting blood glucose test, and the haemoglobin A1c (Hb A1c) test. It is important to note that diagnosing diabetes should not rely solely on using a Hb A1c test. The Hb A1c test can be a useful measure of blood glucose control, but it’s important to remember that it is only an indirect measure of blood glucose control. For some people with diabetes, there may be other conditions that can cause a falsely low or falsely high Hb A1c reading.
What is the Hb A1c test?

The Hb A1c test, or the glycated haemoglobin A1c test, is a blood test that can be taken at any time and is not affected by food. You don’t need to fast before taking the test. It gives an indication as to what your average blood glucose levels have been over the previous three months. It does this by measuring the percentage of haemoglobin, called HbA1, that has a glucose molecule attached to it. After glucose has attached to haemoglobin A1 (HbA1) it is given a new name, Haemoglobin A1c or Hb A1c.
You can use the My Health Explained HbA1c tool to see how your average blood glucose levels are going.
Random blood glucose test
In this test, a blood sample is taken at any random time, regardless of when you last ate. A random blood glucose level of 11.1mmol/L (200mg/dL) or higher can indicate diabetes.
| mmol/L | mg/dL | |
|---|---|---|
| Random blood glucose test | 11.1 mmol/L | 200 mg/dL |
Fasting blood glucose test
A blood sample is taken after an overnight fast. A fast is when you refrain from eating for a period of time. Fasting blood glucose levels less than 5.6mmol/L (100mg/dL) is considered normal. A fasting blood glucose level of 5.6-6.9mmol/L (100-125mg/dL) is considered to be prediabetes, while 7mmol/L (126mg/dL) or higher on two separate tests, is considered diabetes.
| mmol/L | mg/dL | |
|---|---|---|
| Normal | 5.6 mmol/L | 100 mg/dL |
| Prediabetes | 5.6 - 6.9 mmol/L | 100 - 125 mg/dL |
| Type 2 diabetes | 7 mmol/L | 126 mg/dL |
Oral glucose tolerance test
This test is similar to a fasting blood glucose test. In an oral glucose tolerance test, you fast overnight and then a fasting blood sugar level is measured. You then proceed to drink a sugary liquid, and your blood glucose levels are tested periodically for the next two hours.
A blood glucose level less than 7.8 mmol/L (140 mg/dL) is considered normal. A reading of more than 11.1 mmol/L (200 mg/dL) after two hours indicates diabetes, whereas a reading between 7.8 mmol/L and 11.0 mmol/L (140 and 199 mg/dL) indicates prediabetes.
| mmol/L | mg/dL | |
|---|---|---|
| Normal | 7.8 mmol/L | 140 mg/dL |
| Prediabetes, 2hrs later | 7.8 - 11.0 mmol/L | 140 - 199 mg/dL |
| Type 2 diabetes, 2 hrs later | 11.1 mmol/L | 200 mg/dL |
How is type 2 diabetes treated?
Maintaining a healthy weight through a healthy diet and regular physical activity, is not only important in your type 2 diabetes treatment, but it is important for your overall health and well-being.
Below we have briefly outlined how diabetes is treated.
Healthy diet
Understanding what food you can eat and in what quantities can be difficult and there is no set type 2 diabetes diet. It can take some time adjusting to a change in diet, even if they’re only small changes. A healthy diet for people with type 2 diabetes is very similar to a healthy diet of people without type 2 diabetes. The difference is that people with type 2 diabetes mellitus, need to be aware of their carbohydrate intake. You can monitor your carbohydrate intake through carbohydrate counting.
Lose weight if you’re overweight or obese

If you carry weight around your midsection, it can increase your risk of developing type 2 diabetes, especially if it’s visceral fat. Visceral fat is a type of body fat that’s stored around your internal organs, like your liver and intestines. Carrying excess visceral fat has also been associated with an increased risk of developing other health conditions, including heart disease, heart attacks, stroke, and bowel cancer.
Making changes to your diet and increasing your physical activity can help you lose weight, including the nasty visceral fat. Losing even a small amount of weight can improve your health. The study, Effect of Weight Loss With Lifestyle Intervention on Risk of Diabetes, found that in people with prediabetes, for every kilogram lost there was a 16% reduction in risk of developing type 2 diabetes.
You may not realise, but your alcohol and coffee consumption may actually be contributing to weight gain or hindering your weight loss goals. If you are looking to achieve weight loss, it is important to look at what you are drinking, as fruit juice, coffee, and flavoured milks, can impact on your goals just as much as the food you are eating.
Physical activity
Regular exercise has great benefits for everyone, including people with diabetes! Exercise has the ability to lower your blood glucose levels by moving glucose from your bloodstream into your cells where it’s used for energy. Exercising can also increase your sensitivity to insulin, meaning that your body needs less insulin to move glucose from the blood and into the cells.
When exercising, you should aim for at least 30 minutes or more of aerobic exercise on most days of the week. You could even break it up into three lots of 10 minutes and spread it across the day! Remember, if it’s been awhile since you were last active, start slowly and build gradually.

Oral or other medications
There are a number of different types of medications used to treat type 2 diabetes. Sometimes oral medications are given to people with diabetes, for example metformin. Some of these medications can stimulate your pancreas to produce and release more insulin. Other medications can inhibit the production and release of glucose from your liver, which means that you need less insulin. One of the most common medications is metformin and is typically the first medication prescribed to people with type 2 diabetes.
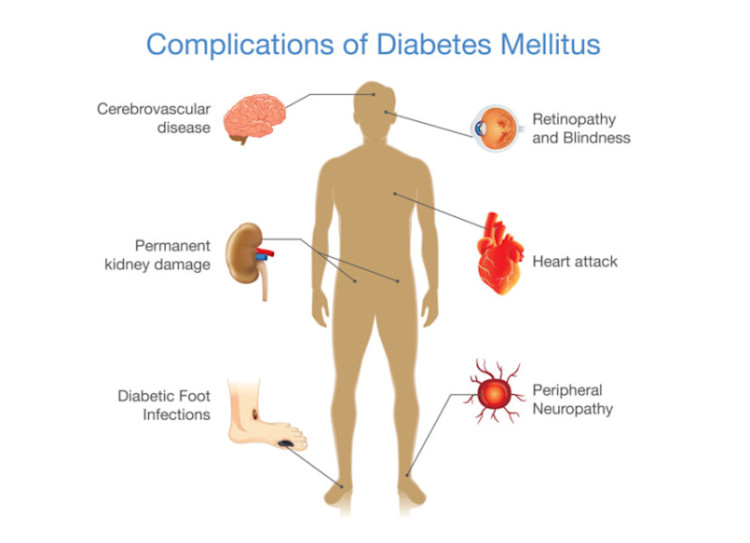
Type 2 diabetes complications
Diabetes is a vascular disease which means it affects blood vessels. Complications in type 2 diabetes can be described as microvascular (small blood vessels) or macrovascular (large blood vessels) complications. Diabetes-related complications occur over time due to persistent high blood glucose levels, high blood pressure, and abnormal cholesterol levels. These complications are serious and can be life-threatening.
Macrovascular complications - Problems with large blood vessels
Macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs. Macrovascular complications include:
- Coronary artery disease which can lead to a heart attack
- Cerebrovascular disease which can lead to a stroke
- Peripheral artery disease which can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity as well as amputations.
Microvascular complications – problems with small blood vessels
Like macrovascular disease, ongoing high blood glucose levels are an important risk factor for the development of microvascular disease in patients with type 2 diabetes. Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Hb A1c and complications in type 2 diabetes
Higher Hb A1c readings are also linked to an increased risk of complications. You can read about Hb A1c and the risk of developing type 2 diabetes complications to learn more.
How do I monitor my diabetes?
Although diabetes is a chronic condition, it is usually controlled through lifestyle changes, medications, and self-care measures. The main goal of diabetes treatment is to keep blood glucose levels within the target and safe range. Self-monitoring blood glucose levels with a glucose meter allows a person to check that their blood glucose levels are within a healthy and safe range.
Monitoring blood glucose levels at home
Monitoring type 2 diabetes is important and this includes blood glucose levels! You may be checking and monitoring your blood glucose levels around four times per day, or even more if you’re using insulin. Careful and regular daily monitoring is the only way to ensure that your blood glucose levels remain within the target range. If you have type 2 diabetes and you aren’t using insulin, you will likely check your blood glucose levels less frequently throughout the day.
Testing blood glucose levels with fingersticks and a glucose meter?
When testing your blood glucose levels through a finger prick test, it’s important to follow the directions of your doctor or the instructions on the glucose meter. It’s important never to share glucose monitoring equipment, as this can lead to infection.

Some general guidelines for testing blood glucose levels include:
- Wash hands with soap and warm water, then dry thoroughly.
- Prepare the lancet device, using a fresh lancet. The lancet will help to draw a small amount of blood from your finger.
- Prepare the glucose meter and test strip.
- Use the lancet to draw a small drop of blood from your finger tip.
- Apply the drop of blood to the test strip in the glucose meter. The result will appear on the display on the meter after several seconds.
- Dispose the lancet in a sharps bin (not in your regular household bin).
Regular blood tests with your doctor
In addition to daily monitoring, you should be having a blood test every three months to check your Hb A1c. Hb A1c is a measure of your average blood glucose level over three months. The Hb A1c test is a good indicator for how well your diabetes treatment plans have been going overall. Your target levels may differ from someone else due to your age or what medications you may be taking to help with your diabetes management.

Monitoring for complications – what do I need to know?
If you have type 2 diabetes, you will require ongoing check-ups to monitor for any diabetes-related complications. This includes regular eye exams with an optometrist and foot exams with a podiatrist. These routine examinations are important as early detection of any microvascular or macrovascular complications can lead to early interventions and treatment that may be able to reverse complications or prevent them from progressing further.
Can I reverse type 2 diabetes?
The short answer is… maybe.
‘Reversing’ is probably not be the best description to use for most people. ‘Slowing the progression’ or a ‘diabetes hiatus’ might be more apt. If we can slow the progression enough, we may actually be able to halt type 2 completely for many years.
Depending on a person’s genetics, weight, motivation, and activity levels, if caught early enough, insulin resistance can be improved, and, the progression of rising blood glucose levels can be slowed.
No matter which stage of diabetes (or prediabetes) you’re at, small (or maybe big) changes can slow down its progression. Lifestyle changes may reduce the number of medications your doctor prescribes in the long term, and hopefully, allow you to live a long and healthy life.
Make the change!
Can I prevent type 2 diabetes?
You may have just found out that you are at risk of developing diabetes. This may be more difficult than you anticipated. However, if you don’t have diabetes yet, this is actually really good news. It means that you can make changes now to prevent or delay developing type 2 diabetes. Making some simple changes now, can have a huge impact on your health for the years ahead, including to reduce your risk of developing diabetes comorbidities; hypertension and dyslipidemia.
So, yes! you can prevent type 2 diabetes. Phew!
What can I do to prevent type 2 diabetes?
There are changes you can make to improve your health and reduce your risk of developing diabetes. These include:
- Eating well
- Moving your body more
- Being a healthy weight
- Setting realistic goals
- Getting support
- Make changes part of your everyday
There is also some evidence that suggests quitting smoking can help to reduce your risk of developing diabetes.
What should I do next?
If you experience any symptoms of type 2 diabetes or you have type 2 diabetes risk factors, it is important to get tested for as soon as possible. Some people are at higher risk and need regular testing. If you are 45 years or older or have other risk factors for diabetes, you will require more frequent testing. By diagnosing and treating the type 2 diabetes early, it means you can decrease the risk of developing diabetes or delay type 2 diabetes complications, for example nerve damage, blindness, and heart disease. It is important to know that diagnosing type 2 diabetes should not rely solely on using a Hb A1c test.
Once you learn what your type 2 diabetes status is, or if you already have type 2 diabetes, the next most important step is to become educated. You can join the 12-week Type 2 Diabetes Program to help you learn how to prevent or delay type 2 diabetes. The program is personalised and tailored, giving you more of the content that you want. The program also helps you to stay motivated and teaches you what changes you need to make. The first week is free and full of helpful and crucial information.
If you would like to be a part of a supportive program, with easy to understand video content covering all aspects of diabetes, join our personalised 12-week program today! Don't forget, when you sign up, you receive the first week free!